Diagnosis
Prostate cancer is a curable disease especially when it is early diagnosed. The high prostate cancer survival rates are based on the efficiency of early diagnosis and the slow-growing characteristic of prostate cancer. Medical advances have led to the development of new, effective methods of prostate cancer diagnosis. These new tests can not only detect the presence of cancerous cells, but also determine the exact location and prognosis of the disease, establishing the stage groups and survival rates.
How prostate cancer is diagnosed
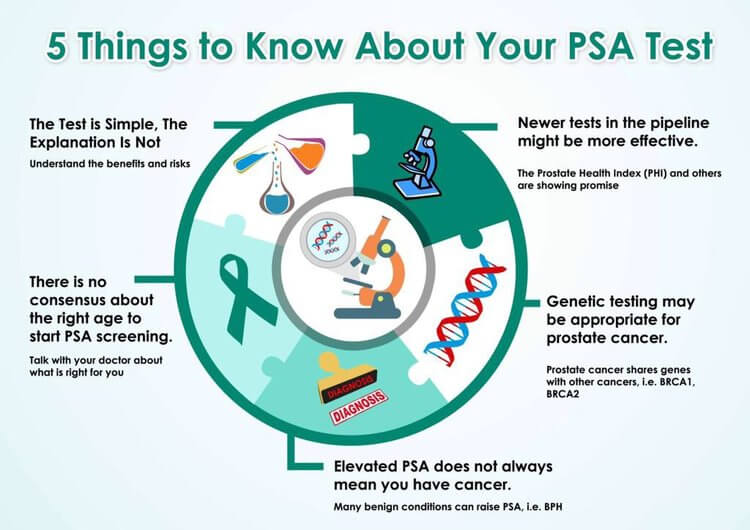
Prostate cancer is diagnosed by means of specific tests, the most used being the PSA test. The Prostate-Specific Antigen Test is a blood test that evaluates the antigen produced by the prostate gland. A PSA level above 4.0 ng/ml may indicate the presence of prostate cancer. However, there are also other methods used for the exact diagnosis of prostate cancer. They include the Digital Rectal Exam, the biopsy, TRUS, MRI, CT, and PT scans, and even PCH blood test and saliva tests for prostate cancer.
PSA test
What is the PSA test?
PSA test is a blood test for prostate cancer, used to monitor the level of prostate-specific antigen (PSA) produced by the prostate gland. The antigen is usually found in the prostate gland and semen, but small amounts of it can also move into the bloodstream and can be measured by the PSA test. Once the PSA grows above a normal 4.0ng/ml, its level is no longer considered normal, but elevated.
When should I have the PSA test?
Since the PSA is a simple blood test, it’s a good idea to get a baseline before the age of 50. With your individual PSA risk factors as a guide, you and your doctor can determine a follow-up screening schedule. The best time for annual PSA screening is between the ages of 55-69. Risk increases significantly after age 65, so diagnosis in this window allows for early, more effective treatment. Screening is still valuable after age 70, depending on overall health. The PSA is not a definite prostate cancer test, but rather an effective early indicator of prostate cancer, infection, or enlargement.
Factors that can influence the PSA level:
- Your age
- The size of your prostate gland
- Whether you’re taking medications that affect PSA measurements, such as finasteride (Propecia, Proscar), dutasteride (Avodart) and even some herbal supplements
Of course, not every PSA needs a biopsy and not every prostate cancer needs treatment. Nowadays, the PSA test has evolved and doctors are looking into more non-invasive diagnosis options after an elevated prostate-specific antigen level, in order to spare men from unnecessary biopsies.
DRE (Digital Rectal Exam)
A digital rectal exam (DRE) is a clinical examination of the prostate gland by way of the rectum, to check for any abnormalities, and is an essential element in screening for prostate cancer. The doctor places a lubricated gloved finger into the rectum to thoroughly examine the prostate. He applies firm pressure to the prostate in order to feel for any abnormalities or enlargement of the prostate.
A digital rectal exam is performed to look for any signs of prostate cancer and, in many instances, is used in conjunction with a prostate-specific antigen test (PSA) to aid in diagnosing the presence of prostate cancer.
It is recommended that men over the age of 50 years old begin screening for prostate cancer. If patients have any additional risk factors for prostate cancer in relation to race (African-American), or have a family history of the disease, then screening can begin as early as 40 years old. The examination will generally only last a few minutes to complete, but can provide valuable information about the prostate condition.
Prostate biopsy
A prostate biopsy is a procedure during which a surgeon removes samples of suspicious tissue from the prostate and sends it to a laboratory in order to be examined under a microscope for signs of prostate cancer. A prostate biopsy may be done in several different ways:
Transrectal – This is done through the rectum and is the most common. Using an ultrasound probe in your rectum, a special needle is inserted into your prostate gland via your rectum to collect prostate tissue samples.
Transurethral – This is done through the urethra using a cystoscope (a flexible tube and viewing device) which is inserted through the opening of the urethra at the tip of the penis. Tissue samples are then collected from the prostate through the scope.
Transperenial – This is performed through the skin between the scrotum and the rectum. A small incision is made in the perineum and a biopsy needle is then inserted through the incision and into the prostate several times, to get samples from different areas of the prostate. Results of a prostate biopsy are usually available within 10 days following the procedure. If cancer cells are present, a grade (Gleason score) will be given, which your doctor will discuss with you. The Gleason score is considered a tool for predicting how aggressive the cancer is. Normal results from a biopsy will suggest that no cancer cells have been found in the prostate, while an abnormal result will indicate that cancer cells are present.
TRUS (Transrectal Ultrasound) and the ultrasound-guided needle biopsy
A transrectal ultrasound (TRUS) is a procedure which utilizes sound waves to create an image of the prostate gland and the surrounding tissue. Generally, the scan requires the insertion of an ultrasound probe into the patient’s rectum. The probe then both sends and receives sound waves through the rectal wall into the prostate gland, which is situated directly in front of the rectum.
Through the prostate ultrasound, the doctor collects a sample of cells or tissues from the abnormality, to be examined under a microscope. This way, cancerous cells can be detected in the prostate.
“The problem of using TRUS biopsy is that it only samples the lower portion of the prostate, representing only about 1% of the prostate tissue when searching for prostate cancer. It uses a needle to collect twelve random samples within twelve cores of the prostate,” said Dr. David Samadi.
“However, almost 30% of cancers are found outside of this area. This means that even if the biopsy is negative for finding cancer, there is still the possibility that the TRUS biopsy may have missed pockets of undetected disease.”
Regarding the use of invasive biopsies in the process of prostate cancer diagnosis, Dr. David Samadi stated: “Anytime there are more invasive procedures such as a biopsy using needles involved in detecting prostate cancer, it is always a concern for the man having the procedure done. There are concerns of pain, infection and bleeding that can be distressing to a man. In addition, a biopsy is not as accurate in diagnosing prostate cancer, which can lead to false positives when the cancer is too slow-growing to be harmful or not even present.” As such, less invasive methods for diagnosis have registered an increase in popularity.

Non-invasive diagnosis methods – Imaging tests
For a long time, most prostate cancer diagnosis have been discovered with the biopsy procedure. Doctors analyze the tissue and are able to determine the clinical pathological characteristics of the cells. The issue with this procedure is that it’s invasive and very uncomfortable for the patients and, most often, the results are negative. The patients either do not have cancer or have to repeat the procedure, as there is other clinical evidence of neoplasia. Therefore, other non-invasive methods of cancer detection have been developed, that are able to detect cancer at molecular levels, making it possible to determine a correct staging for the disease.
Magnetic Resonance Imaging (MRI) is used in radiology to recreate detailed pictures of the prostate and the nearby tissues. The procedure is fast, safe, non-invasive and does not use X-rays or ionizing radiation. The images are generated with the help of magnetic fields, magnetic field gradients and radio waves. It is used to check for cancerous cells within the prostate and to determine the aggressiveness of the cancer. MRI scans are usually performed before a biopsy, thus avoiding many unnecessary painful screening procedures. If something unusual is detected, by means of the MRI scan the doctor can determine the exact location from where to take biopsy samples.
MRI guided fusion biopsy provides additional advantages over the classic MRI scan or TRUS. It can fuse together real-time ultrasound images of the prostate, allowing more accurate and precise identification of suspicious lesions which may not have been found using traditional transrectal ultrasound. “Using MRI-US guided fusion biopsy has a 30-40% better chance of finding cancer than just using TRUS guided biopsy. It only takes about 15 minutes and can be done in the office.”, said Dr. David Samadi.
The MRI-US guided fusion biopsy also plays a valuable role in evaluating low-risk patients with active surveillance and it can identify more aggressive cancers needing to be removed quickly, in order to spare a patient’s quality of life and prevent metastasis.
A CT scan uses X-rays to create detailed images of the prostate. This test is often needed if the tumor is likely to have spread out of the prostate. CT scans provide valuable information about the prostate surrounding tissues and whether the lymph nodes have been affected.
A PET scan is usually combined with a CT scan to improve the quality of the images. PET scans employ a tracer drug called Axumin. Attached to it is a radioactive tracer, fluorine-18. The PET/CT scanners detect the energy created by the radioactive tracer and it is automatically converted into an image on a computer. PET/CT scans have improved the quality of the care provided, especially for recurrent cancers.
Prostate cancer can metastasize to the bones and the doctor may perform a bone scan to detect whether the cancer has spread outside the gland. The automated Bone Scan Index (aBSI) uses artificial neural networks to detect metastatic hot spots and classify them as malignant or benign.
New genetic tests for prostate cancer
A ground-breaking study published by the Prostate Cancer Foundation (PCF), reported that one in nine (12%) men with metastatic prostate cancer carry inherited mutations in DNA damage repair (DDR) genes, that most likely caused their disease. Genetic testing helps identify men with very high risk and, if found to be positive, family members would be encouraged to seek genetic counseling.
Our genetic makeup can be found in our saliva. Cancer occurs when genes are combined in a different, abnormal way. This test looks for these combinations or variations that are considered risk signatures, or biomarkers, for prostate cancer. Now, a relatively simple 10-minute saliva-based DNA test can also identify variations on genes that identify men who are at the highest risk of developing prostate cancer.
These prostate cancer tests help both the patient and the doctor have a clear vision about the prostate condition, the presence of cancer, its aggressiveness, prognosis and whether it is low-risk or high-risk. The results of the PSA test, DRE, biopsy or other tests are combined and provide information about the stage of cancer, which is vital in determining the right treatment. The next section discusses the stages of prostate cancer and how to understand your results.
Bibliography
- Prostate Cancer in Primary Care, PubMed Abstract, Web, 10 Aug 2018
- Global Advances in Prostate Cancer Diagnosis, PubMed Abstract, Web, 22 Apr 2013
- Advances in Prostate Cancer Research, National Cancer Institute, Web, 2 MAy 2019
- Prostate Cancer Diagnosis and Staging, Medscape, Web, 14 Jan 2019