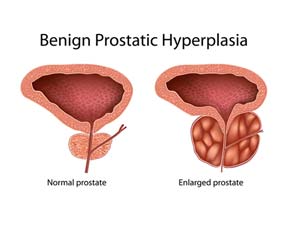
In addition to prostate cancer there are two benign prostate conditions that have symptoms that are similar to prostate cancer. The first in this brief series of blogs I will discuss is about benign prostatic hyperplasia. Benign prostatic hyperplasia or BPH as it is commonly abbreviated is the noncancerous enlargement of the prostate gland and is an occurrence most common in older men aged 40 to 70. When the prostate starts to grow in size, the gland will begin to press against and squeeze the urethra. The wall of the bladder will gradually become thicker because of the increased pressure. Inevitably, the bladder will significantly weaken and lose the capacity to completely empty urine from the bladder. The narrowing of the urethra in addition to the inability to completely empty the bladder will attribute to many of the issues connected with benign prostatic hyperplasia.
Causes/Symptoms
Despite past and ongoing research the exact cause for BPH is not fully understood. Common causes that are regularly attributed to BPH include: aging, family history, various medical conditions (obesity, type 2 diabetes), inadequate amount of physical activity and hormonal changes. For the majority of men who have BPH many will not exhibit any discernible signs or symptoms of the condition. Although when symptoms do begin to occur they can range from mild to severe and the severity of the symptoms aren’t necessarily associated with the amount of prostate growth. For example, a patient with a significant amount of prostate enlargement may only have mild symptoms while another patient with minimal prostate growth will have a greater severity in their symptoms.
Symptoms include:
- Weak urinary stream
- Difficulty starting urination
- Frequently needing to urinate
- Inability to empty bladder completely
- Leaking or dribbling of urine
- Repeated urinary tract infections
Diagnosing BPH
Your doctor will begin by asking you a series of detailed questions in relation to your symptoms, evaluate your complete medical history and perform a full physical examination. Some of the diagnostic procedures used to diagnose BPH might include:
Digital Rectal Exam (DRE): Is a procedure in which a doctor will insert a lubricated gloved finger into the rectum to examine the prostate gland for abnormalities, prostate enlargement and any signs of cancer.
Urinary Flow Test: Your doctor will have you urinate into a repository attached to a device designed to measure the strength and volume of your urine flow. Results help to determine the severity of your condition.
Cystoscopy: An optic instrument with a lighted tip called a cystoscope is inserted through the urethra to thoroughly examine the bladder and urinary tract. Your doctor will be look specifically for any obstructions or abnormalities.
Treatment options
Treatment of BPH will depend on a number of variables which will range from the age of the patient, overall health, and the severity of their symptoms. If the symptoms are mild in nature, a patient can choose to forego treatment temporarily and essentially monitor the progression of their symptoms with their doctor through active surveillance. Often times patients with mild symptoms may only require simple lifestyle changes in order to improve their prognosis. For patients with more severe symptoms there are a number of options, some of which include:
Medications: Alpha Blockers are commonly used to treat mild to moderate symptoms of BPH. An alpha blocker works by relaxing the muscles in the bladder making it easier for the patient to urinate. Several of these medications include: alfuzosin (Uroxatral), Doxazosin (Cardura), tamsulosin (Flomax) and terazosin (Hytrin).
Surgery: Surgery is perhaps one of the best ways to effectively treat BPH but does carry a small risk of potential side effects such as erectile dysfunction. The most commonly used surgical treatment for BPH is transurethral resection of the prostate (TURP). This procedure is performed by inserting a scope through the penis and removing excess tissue blocking the urethra. Because the procedure is one that doesn’t require the use of an incision, the risk of infection is greatly reduced.
While benign prostatic hyperplasia (BPH) isn’t necessarily life threatening, symptoms should never be ignored as they can lead to other serious conditions. If you are unsure if you may be experiencing symptoms of BPH contact our office to set up a consultation. Take the first steps to improving the quality of your life.